Throughout October, we’ll be highlighting our SLOSS work to address health inequities in areas that disproportionately affect Black communities. We’ll focus on blood-borne viruses, renal, cardiac, and sickle cell disorder and what we’re doing to help.
Blood-borne viruses
People with HIV who take HIV medicine (called antiretroviral therapy, or ART) as prescribed can get and keep an undetectable viral load – meaning they will not transmit HIV to their HIV-negative partners.
That’s why our HIV re-engagement programme is so important. We’re working to reconnect individuals back into care, ensuring they receive the support and treatment they need.
Already the team have re-engaged 350 people in south east London, giving them the chance to take control of their health and avoid potentially devastating illness.
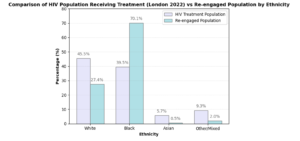
Of those people we have re-engaged into HIV care, 70% are from Black communities. This is a much higher proportion than the overall population of people living with HIV. See our graph below and contact us for details on our south east London re-engagement evaluation.
Sickle cell disorder
Sickle cell is a lifelong inherited condition that changes the shape of red blood cells, leading to blockages in blood vessels. Common symptoms include anaemia, painful episodes (known as crises), and an increased risk of serious infections. While sickle cell can affect anyone, it primarily affects individuals from African and Caribbean backgrounds.
The “No One’s Listening” report, published in 2021, highlights evidence of inadequate care in hospital wards and emergency departments for people living with sickle cell disorder. It raised concerns about negative attitudes towards individuals with sickle cell, suggesting these attitudes may stem from racial biases, a lack of awareness, limited education, and insufficient resources for sickle cell care.
During Black History Month, we want to showcase some of the work being done to address these health inequalities and improve care for those living with sickle cell disorder in south London. Throughout the week, we’ll be sharing updates on the progress being made in community care, digital care plans, and within emergency departments.
Sickle cell disorder: ACT NOW sickle cell acronym
The ACT NOW sickle cell initiative, is part of an NHS England campaign to ensure rapid and effective care during a sickle cell crisis. The acronym has been co-developed by clinicians, experts, and people living with sickle cell disorder. It provides clear clinical guidance and is now available across hospitals in England.
The initiative addresses the challenges identified in the “No One’s Listening” report and aims to improve patient outcomes and experiences. By ensuring healthcare teams are trained and equipped to respond swiftly to sickle cell crises, the NHS is helping to close the gap in health inequalities with sickle cell primarily affecting Black African and Caribbean communities.
Through NHS England‘s collaboration with organisations like the Sickle Cell Society, and with a growing number of sites evaluating its impact, ACT NOW is crucial for delivering inclusive, equitable care to patients across the country.
Learn more and access resources on the NHS England website to support the rollout of the ACT NOW acronym across England.
Sickle cell disorder: Universal Care Plan
The Universal Care Plan (UCP) is a digital patient care record. It is currently being expanded, across all of London, to meet the needs of those with sickle cell disorder across all settings of care, which means being able to access digital care records online. 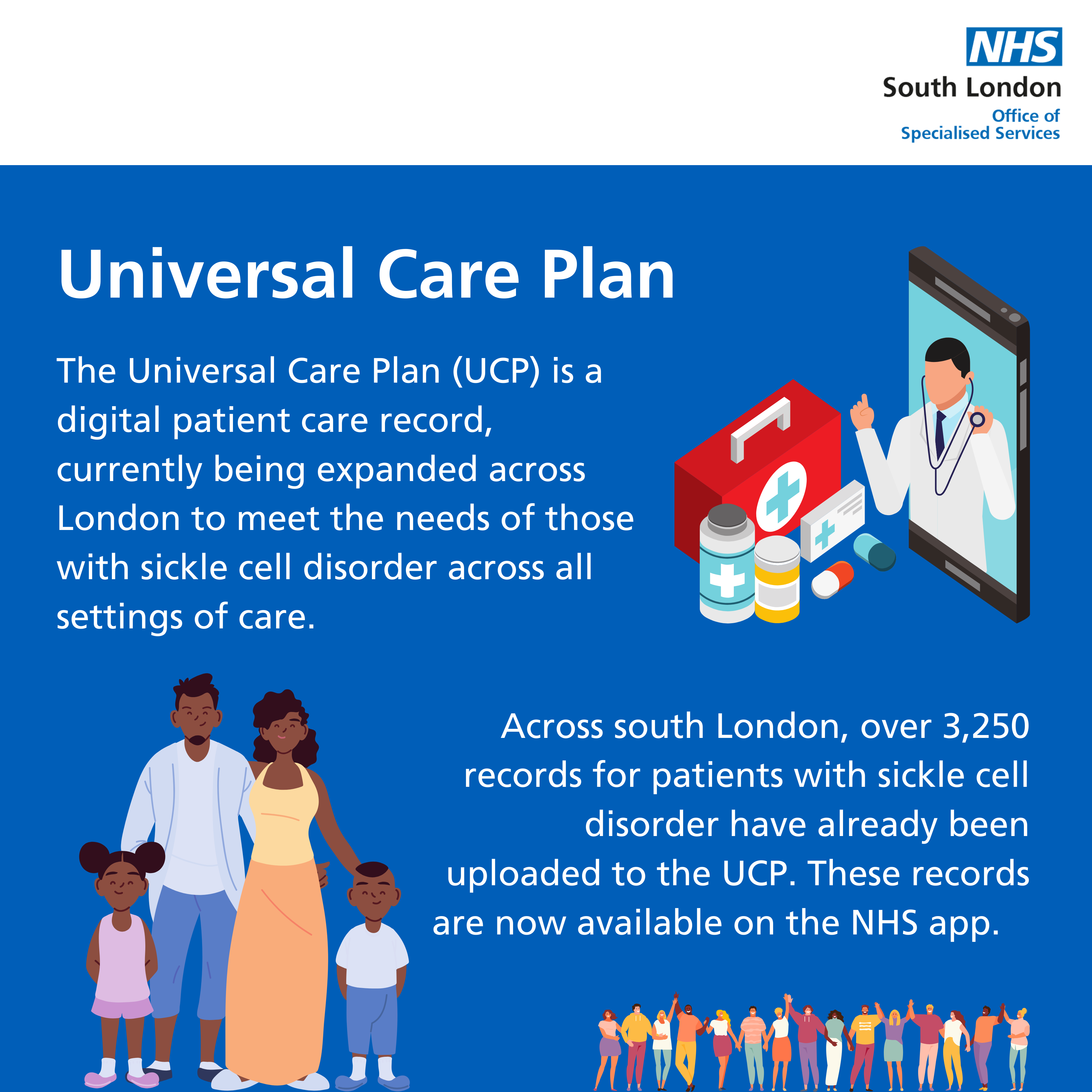
The UCP has been designed to improve handover between emergency and acute care for sickle cell pain crises. The new template offers clinical guidance and personalised, individualised care plans, helping to reduce unnecessary hospital admissions, delays in treatment, and ensures patients receive care at the right time and place.
With consistent information sharing between services, it will reduce clinical conflict and support better communication, inclusion, and accessibility for patients, allowing them to be actively involved in their care.
Across south London, over 3,250 records for patients with sickle cell disorder have already been uploaded to the UCP. People living with sickle cell can now personalise their care by registering their treatment preferences directly on the NHS app, ensuring future care is tailored to their needs.
This Black History Month, we recognise the importance of initiatives like the UCP in driving health equity and improving outcomes for communities affected by sickle cell disorder.
Patients: Find out more in the patient flyer and visit the UCP website.
Healthcare professionals: Get trained on the UCP through the UCP website, NHS Learning Hub, and the UCP training YouTube video for sickle cell.
Sickle cell disorder: Peer mentoring programme and community services
The Sickle Cell Society led children and young people peer mentoring programme is a powerful London-wide initiative which pairs young people, aged 10-24, living with sickle cell with mentors who have first-hand experience living with the condition.
This Black History Month, we celebrate the importance of initiatives like these in empowering Black communities and addressing health inequalities. By offering tailored advice, emotional support, and guidance the programme helps young people understand and manage their condition, and navigate their transition to adult services, ensuring they feel heard and understood.
The children and young people peer mentoring programme recently appeared on ITV, where Rachel, one of the south east London mentors, and Marilen, one of her mentees, shared about their experience on the scheme. Marilen said: “I love the fact that this programme has mentors that actually have sickle cell; it’s so relatable! When I met my mentor, we sat and spoke for hours and I’ve never felt so satisfied. I finally felt heard, and it was so reassuring to know that I’m not the only one suffering.” Read more about the ITV interview on the South East London ICS website.
This programme is part of a wider initiative to improve community services for people living with sickle cell disorder. The enhanced services will provide greater holistic support for people living with sickle cell. Each area is tailoring these services to best suit the care of their patients. If you would like to find out more about what is happening in your area, you can reach out to your local red cell care team.
You can ask your nurse, doctor or parent/guardian to fill out the online Sickle Cell Society form to register your interested in getting involved in the programme.
If you have any general enquiries or are interested in becoming a mentor, you can email mentors@sicklecellsociety.org.
Heart valve disease
Within the South London Cardiac ODN, we’re working to address inequalities in heart valve disease. The report “Addressing inequalities in heart valve disease“, documented key findings and recommendations, as featured in the King’s Fund report, “Cardiovascular disease in England”.
We’re taking action to create a more equitable healthcare system for all.
Multiple long-term conditions
Multiple long-term conditions: Background
This Black History Month, we want to talk about the health inequalities found among people living with multiple long-term conditions, and how services can provide support. It has been found that people from disadvantaged backgrounds, minority ethnic groups and those with serious mental illness are at the greatest risk of developing multiple long-term conditions. People on the lower incomes are four times more likely to have multiple long-term conditions than people on the highest incomes.
It is shown that people from ethnic minority groups, including those from Black African and Caribbean backgrounds, are at a significantly increased risk of having multiple long-term conditions, in particular diabetes, chronic pain and cardiovascular disease, and are also more likely to develop conditions earlier. In south east London, 40% of the population living with chronic kidney disease, cardiovascular disease and diabetes are from minority ethnic groups, which is disproportionate to the population in south east London.
Research suggests that underlying drivers of this may include health-related behaviours, lack of access to material resources and the psychological response to social inequality. Individual experiences of health services often differ significantly, where the needs of disadvantaged groups are often neglected or even made worse by services’ responses.
We have a responsibility to best tackle these inequalities and improve health outcomes for those who are most affected. Later this week, we will look at services that are being offered to help confront and tackle health inequalities, including more holistic and integrated care models that are being implemented across south London. Let’s work together to address these challenges and support equitable healthcare for all. Learn more about the health inequalities found among people living with multiple long-term condition in the National Institute for Health and Care Research (NIHR) report.
Multiple long-term conditions: South east London multi-morbidity model of care

People living with multiple long-term conditions often experience a lack of coordination, with multiple appointments in multiple settings, and a lack of personalisation or holistic approach. As explored earlier this week, people from disadvantaged backgrounds, minority ethnic groups and those with serious mental illness are at a greater risk of developing multiple long-term conditions and facing health inequalities.
With over 46,700 in south east London with identified chronic kidney disease (CKD), many with additional long-term conditions, and over 350,000 at heightened risk of developing CKD, there is significant need for transformation of services for those living with multiple long-term conditions, and those who face significant inequalities. In addition, 40% of the population living with CKD, cardiovascular disease and diabetes are from minority ethnic groups, which is disproportionate to this population in south east London.
In response to this, the South East London Integrated Care System has been working with Primary Care Networks, community staff and secondary care staff to set up a new and innovative model of care. Currently in seven Integrated Neighbourhood Teams across south east London, the model will use existing clinical and non-clinical resources to build teams that provide holistic and joined-up care in the community. This will support the south east London population to have better health outcomes, be healthier for longer and avoid end stage kidney disease and dialysis, leading to a more sustainable and effective model of care.
Chronic kidney disease
This Black History Month, we’re spotlighting the urgent need to address health inequalities, particularly in Chronic Kidney Disease (CKD). In the UK, people from Black and South Asian communities are 3-5 times more likely to need dialysis, and those from lower-income backgrounds experience faster progression to kidney failure.
Kidney Research UK proposes three interventions to improve outcomes from CKD:
- Early diagnosis in underserved populations with community outreach
- Improved management in line with clinical guidelines
- Use of SGLT2i inhibitors to reduce heart attacks, strokes and progression to end stage kidney disease.
In south east London, we’re embedding vital recommendations from Kidney Research UK, into our multi-morbidity model of care, whilst working collaboratively, to enhance the health of the local population. We are doing this through:
-
Engaging with communities and proactively screening for chronic kidney disease in high risks groups.
-
Using remote testing with Healthy.io, to increase accessibility and convenience for high risk communities
-
Carrying out quality improvement work to find sustainable working models to implement CESEL CKD guidelines, prioritising those in CORE20PLUS5 groups.
-
Upskilling allied health professionals, and pharmacists to generate necessary capacity within primary care.
This would not be possible without the joined up effort of South East London ICS, with King’s College London, the London Kidney Network, Clinical Effectiveness South East London, neighbourhood community organisations, and the Hidden CKD project.



